- Updated on September 11, 2020
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
- Medically Reviewed by Naziliya Rakhimova, MD
Heavy Breathing: How People Die Due to Diseases
“…Death consists of the passing out of the air. It is, therefore, necessary to restrain the breath.”
Hatha Yoga Pradipika, (15th century)
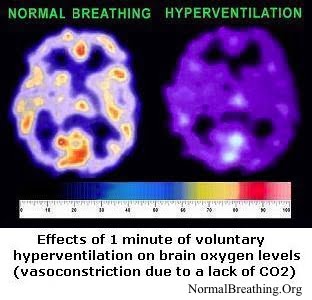 It is a normal clinical finding that with approaching death, breathing becomes faster and deeper, while oxygen levels in the brain and other cells becomes lower and lower. Separate web pages on this website have medical references that confirmed very high respiratory rates (labored breathing) in terminal cancer, last stages of HIV-AIDS, cystic fibrosis, and other conditions. (By the way, in the 1950’s, observations of breathing patterns in dying hospital patients led to the discovery of the Buteyko breathing method: slow down your heavy breathing back to the medical norm.)
It is a normal clinical finding that with approaching death, breathing becomes faster and deeper, while oxygen levels in the brain and other cells becomes lower and lower. Separate web pages on this website have medical references that confirmed very high respiratory rates (labored breathing) in terminal cancer, last stages of HIV-AIDS, cystic fibrosis, and other conditions. (By the way, in the 1950’s, observations of breathing patterns in dying hospital patients led to the discovery of the Buteyko breathing method: slow down your heavy breathing back to the medical norm.)
 Many studies commented on and measured effects of heavy breathing on the health status of different groups of patients.
Many studies commented on and measured effects of heavy breathing on the health status of different groups of patients.
For example, 29 patients with severe liver damage (in most cases due to deadly metastatic cancer or cirrhosis of the liver) all had low arterial carbon dioxide, while for 25 patients “it was also clinically evident that respiratory exchange was increased markedly” (p.762, Wanamee et al, 1956).  Thus, hyperventilation or heavy breathing was visually observed by the authors of this publication, Respiratory alkalosis in hepatic coma. They also found that very heavy breathing led to severe electrolyte abnormalities. These abnormalities included decreased sodium ions and increased chloride ions in the blood. Abnormally high lactic and pyruvic acid concentrations were other frequent effects.
Thus, hyperventilation or heavy breathing was visually observed by the authors of this publication, Respiratory alkalosis in hepatic coma. They also found that very heavy breathing led to severe electrolyte abnormalities. These abnormalities included decreased sodium ions and increased chloride ions in the blood. Abnormally high lactic and pyruvic acid concentrations were other frequent effects.
 Blood gases and respiratory patterns provided accurate information for survival prognosis in acute cerebrovascular accidents. When these parameters were normal, patients survived. Out of 11 hyperventilating patients with less than 35 mm Hg aCO2 (arterial carbon dioxide), only one survived (Rout et al, 1971).
Blood gases and respiratory patterns provided accurate information for survival prognosis in acute cerebrovascular accidents. When these parameters were normal, patients survived. Out of 11 hyperventilating patients with less than 35 mm Hg aCO2 (arterial carbon dioxide), only one survived (Rout et al, 1971).
The same conclusion (regarding aCO2 and survival prognosis) was made for head injuries (Huang et al, 1963; Vapalanti & Trouph, 1971).
Death and heavy breathing
Summarizing the results of these works and their connection with brain dysfunction, Dr. Plum wrote,
“The combination of hyperpnoea [increased breathing] with an elevated pH and a subnormal or moderately low oxygen tension occurs in many serious illnesses that entirely spare the brain.
These include the alveolar-capillary block of diffuse pulmonary carcinomatosis; heart failure; advanced cirrhosis, with or without hepatic coma; acute pulmonary infarction; and many others, including the cryptic pulmonary congestion that accompanies most serious disease in the obtunded and elderly” (Plum, 1972).
 Interestingly, all above-mentioned effects (low carbon dioxide concentration, elevated pH, and hypoxia or low O2 pressure in cells) quoted by Dr. Plum are caused by heavy breathing.
Interestingly, all above-mentioned effects (low carbon dioxide concentration, elevated pH, and hypoxia or low O2 pressure in cells) quoted by Dr. Plum are caused by heavy breathing.
As a result, one can conclude that labored breathing is a normal feature of these severe diseases.
When suffering various serious health problems (heart disease, diabetes, cancer, AIDS, etc.) the patient’s life is very frequently threatened, not by the main health problem, but by complications and infections, such as in the case of bacteremic shock.
Analyzing a group of patients initially diagnosed with arteriosclerotic heart disease, cerebrovascular insufficiency, diabetes, arthritis, several forms of cancer, fatty liver, and alcoholism, one study showed that complications due to pathogenic microorganisms in the blood caused 46 deaths in 50 patients (Winslow et al., 1973).
Pneumonia and urinary tract infections were the foci of pathogenic microorganisms. Now we may ask the following: what was observed with their breathing when not only a part of the organism but even the blood was polluted with pathogens? All 50 patients, according to a table accompanying this article, had very disturbed blood gases corresponding to very labored breathing.
 Dr. Simmons and his colleagues wrote an article “Hyperventilation and respiratory alkalosis as signs of gram-negative bacteremia” (bacteremia being the presence of bacteria in the blood). This extract is from the beginning of their abstract:
Dr. Simmons and his colleagues wrote an article “Hyperventilation and respiratory alkalosis as signs of gram-negative bacteremia” (bacteremia being the presence of bacteria in the blood). This extract is from the beginning of their abstract:
“Visible hyperventilation was observed clinically in patients with Gram-negative bacteremia. Eleven patients with Gram-negative infections and either proved or probable bacteremias were therefore studied to see if hyperventilation might be a common response to such bacteremia.
In every case, there was laboratory evidence of hyperventilation, and in 8 cases the hyperventilation was visible to the observer. Since only patients were studied who had no other cause for increased ventilation, this appears to be a primary response to the bacteremia…” (abstract, Simmons et al, 1960).
 Another group of US medical professionals found that the degree of heavy breathing has a strong correlation with overall mortality (Mazarra et al, 1974). Heavier breathing indicated smaller chances of survival. Here is what they wrote in their scientific abstract:
Another group of US medical professionals found that the degree of heavy breathing has a strong correlation with overall mortality (Mazarra et al, 1974). Heavier breathing indicated smaller chances of survival. Here is what they wrote in their scientific abstract:
Through a retrospective review of the randomly selected hospital records of 114 patients, we defined four groups based upon arterial carbon dioxide tension (PaCO2) and mode of ventilation.
Group I, with a PaCO2 of 15 mm Hg or less, consisted of 25 patients with an overall mortality of 88 percent. Group II, with a PaCO2 of 20 to 25 mm Hg, consisted of 35 patients with a mortality of 77 percent. Group III, with a PaCO2 of 25 to 30 mm Hg, consisted of 33 patients with a mortality of 73 percent, and Group IV, with a PaCO2 of 35 to 45 mm Hg, consisted of 21 patients with a mortality of 29 percent (p<0.001). Shock and sepsis were most common in group I patients (abstract, Mazarra et al, 1974).
 This article indicated that the names of the most common diseases to occur in all 4 groups of people were cerebrovascular disease, hepatic coma, bronchopneumonia, and arteriosclerotic heart disease.
This article indicated that the names of the most common diseases to occur in all 4 groups of people were cerebrovascular disease, hepatic coma, bronchopneumonia, and arteriosclerotic heart disease.
The analysis of Western medical literature suggests that many critically ill patients die in conditions of heavy and deep breathing.
Up to 90% of deaths in the severely sick take place when breathing becomes progressively heavier and deeper, while the CP gradually approaches zero.
A review of these medical professional studies indicates that critically ill patients usually have very low carbon dioxide level due to severe hyperventilation.
Heavy breathing or even panting at rest (dyspnea) of such patients usually corresponds to minute ventilation of 20-25 l/min or more, while body-oxygen content is less than 10 s. Their typical breathing pattern is shown below.
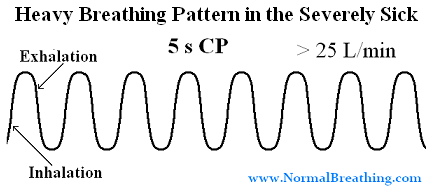
Fig. Heavy breathing pattern of critically ill people: fast labored breathing with very low cell oxygenation (less than 10 s for the body oxygen test).
This YouTube video “Hypocapnia, Respiratory Alkalosis: Key Causes of Deaths In the Sick” provides the same information about hypocapnia and respiratory alkalosis as common causes of mortality in the severely and critically ill people.
Resources
– YouTube video clip “Sleep Heavy Breathing Effect (Buteyko Technique)”
There is one page on this site that quotes over 10 clinical studies that discovered that people with chronic diseases have highest chances of death (highest mortality), as well as highest chances of acute attacks (exacerbations due to heart attacks, strokes, seizures, etc.) during the same part of the day. The link to this page is provided as your bonus content right below here.
Morning Heavy Breathing Effect – Severely sick people with asthma, COPD, heart disease, coronary artery spasms, stroke, epilepsy seizures, and many other conditions have highest mortality rates (largest death toll) during early morning hours.
[/sociallocker]
References (Heavy Breathing in the Critically Ill and Terminal Patients)
Huang CT, Cook AW, Lyons HA, Severe cranio cerebral trauma and respiratory abnormalities, Arch Neurol 1963, 9: p. 545-554.
Mazarra JT, Ayres SM, Grace WJ, Extreme hypocapnia in the critically ill patient, Amer J Med Apr 1974, 56: p. 450-456.
Plum F, Hyperpnea, hyperventilation and brain dysfunction, Annals of Intern Med 1972, 76: p. 328.
Rout MW, Lane DJ, Wolliner L, Prognosis in acute cerebrovascular accidents in relation to respiratory pattern and blood gas tension, Br Med J 1971, 3: p. 7-9.
Simmons DH, Nicoloff J, Guze LB, Hyperventilation and respiratory alkalosis as signs of gram-negative bacteremia, J Amer Med Assoc 1960, 174: p. 2196-2199.
Vapalanti M & Troup H, Prognosis for patients with severe brain injuries, Br Med J 1971, 3: p. 404-407.
Wanamee P, Poppel JW, Glicksman AS, Randall HT, Roberts KE, Respiratory alkalosis in hepatic coma, Arch Intern Med 1956, 97: p. 762-767.

