- Updated on November 1, 2020
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
Oxygen Bar Review: Brain O2 Effects
 An oxygen bar is a place that sells nearly-pure oxygen for public use (no prescription required). Many people believe that oxygen bar can increase oxygen levels in the brain and body cells. This post reviews the real effects. Can breathing pure oxygen in an oxygen bar increase body and brain oxygenation improve health and well-being?
An oxygen bar is a place that sells nearly-pure oxygen for public use (no prescription required). Many people believe that oxygen bar can increase oxygen levels in the brain and body cells. This post reviews the real effects. Can breathing pure oxygen in an oxygen bar increase body and brain oxygenation improve health and well-being?
It was thought “yes” by US scientists in the 1960’s when they were preparing the first American outer space rockets and astronauts. In fact, pure oxygen was used during the first three Apollo missions. Thus, first US astronauts were among primary clients of the “oxygen bar”. At this time, they had not realized yet that pure oxygen is toxic for mammals.
The Soviets were much smarter. The effects of an oxygen bar and other air mixtures were investigated in the 1960’s during highly confidential projects led by leading Soviet physiologist Konstantin Buteyko, MD, Ph.D., who was the manager of the Respiratory Laboratory in Novosibirsk.
 As a result of his discoveries, Soviets still use for their spaceships the ideal air composition, which includes about 10-12% O2, 2% CO2 and 86-88% nitrogen. The ideal air has about twice less oxygen than air at sea level modeling at high altitude, while additional CO2 is the key factor that increases body and brain O2.
As a result of his discoveries, Soviets still use for their spaceships the ideal air composition, which includes about 10-12% O2, 2% CO2 and 86-88% nitrogen. The ideal air has about twice less oxygen than air at sea level modeling at high altitude, while additional CO2 is the key factor that increases body and brain O2.
What is the effect of breathing pure oxygen, like in the case of having an oxygen bar? During very small and slow normal diaphragmatic breathing at rest, blood oxygenation is about 98-99%.
Therefore, an oxygen bar would not increase O2 levels in the arterial blood to any significant degree. However, not all oxygen in the blood is bound with hemoglobin cells. About 2% of the total amount of oxygen in the blood is dissolved in plasma in the same way as it can be dissolved in water as free oxygen.
This is the mechanism of how and why pure oxygen saves lives of critically-ill people. The problem appears when pure O2 is used for hours or even days. Due to its highly-reactive chemical nature, pure oxygen destroys cells in the lungs and blood vessels. This causes oxidative stress, generation of free radicals and intensification of respiration (heavier or faster breathing, which is called hyperventilation).
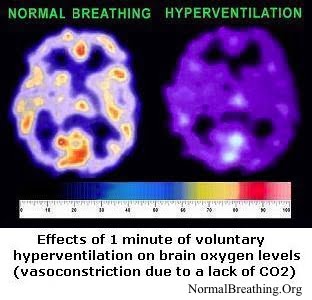
Hyperventilation causes CO2 losses, the immediate spasm of blood vessels, and a suppressed Bohr effect. These factors dramatically reduce O2 delivery to the brain and all other vital organs.
The image on the left shows a typical result, while there are hundreds of other studies that made the same conclusion: lowered CO2 reduces O2 delivery to cells. You can find exact details and references on other pages of this site (see links at the bottom of this page).
There is also a reference below related to the effect of an oxygen bar on brain O2 content. It is called the “hyperoxic brain” effect meaning that breathing hyperoxic mixtures (with more than 21% O2) causes reduced brain O2 levels.
Why oxygen bar idea is popular
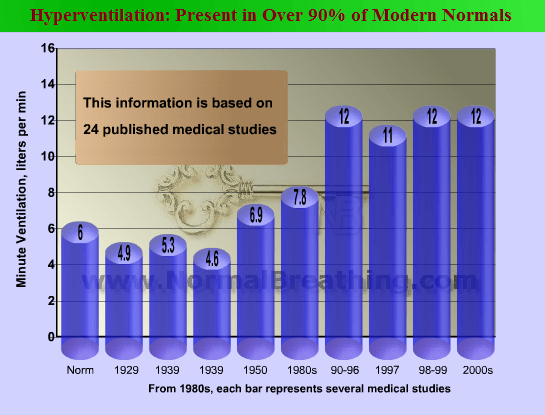
Modern people breathe about 2-3 times more air than people breathed during the first decades of the 20th century. Therefore most contemporary people suffer from the reduced brain and body O2 levels. It is, therefore, logical that many people like the idea of an oxygen bar and search for similar methods to increase their body and brain oxygenation, but there are simple natural alternatives that work far better for increasing body and brain O2 and improving one’s health.
References
Macey PM, Woo MA, Harper RM, Hyperoxic brain effects are normalized by addition of CO2, PLoS Med. 2007 May; 4(5): e173..
Department of Neurobiology, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, California, United States of America.
BACKGROUND:
Hyperoxic ventilation (>21% O2) is widely used in medical practice for resuscitation, stroke intervention, and chronic supplementation. However, despite the objective of improving tissue oxygen delivery, hyperoxic ventilation can accentuate ischemia and impair that outcome.
Hyperoxia results in, paradoxically, increased ventilation, which leads to hypocapnia, diminishing cerebral blood flow and hindering oxygen delivery. Hyperoxic delivery induces other systemic changes, including increased plasma insulin and glucagon levels and reduced myocardial contractility and relaxation, which may derive partially from neurally mediated hormonal and sympathetic outflow.
Several cortical, limbic, and cerebellar brain areas regulate these autonomic processes. The aim of this study was to assess recruitment of these regions in response to hyperoxia and to determine whether any response would be countered by addition of CO2 to the hyperoxic gas mixture.
METHODS AND FINDINGS:
We studied 14 children (mean age 11 y, range 8-15 y). We found, using functional magnetic resonance imaging, that 2 min of hyperoxic ventilation (100% O2) following a room air baseline elicited pronounced responses in autonomic and hormonal control areas, including the hypothalamus, insula, and hippocampus, throughout the challenge.
The addition of 5% CO2 to 95% O2 abolished responses in the hypothalamus and lingual gyrus, substantially reduced insular, hippocampal, thalamic, and cerebellar patterns in the first 48 s, and abolished signals in those sites thereafter. Only the dorsal midbrain responded to hypercapnia, but not hyperoxia.
CONCLUSIONS:
In this group of children, hyperoxic ventilation led to responses in brain areas that modify hypothalamus-mediated sympathetic and hormonal outflow; these responses were diminished by addition of CO2 to the gas mixture. This study in healthy children suggests that supplementing hyperoxic administration with CO2 may mitigate central and peripheral consequences of hyperoxia.