- Updated on October 14, 2020
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
- Medically Reviewed by Naziliya Rakhimova, MD
Breathing pattern for maximum brain oxygenation
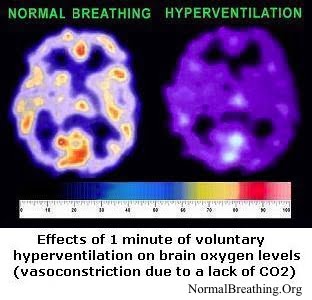 Our breathing pattern has profound effects on the brain. Unnoticeable changes in breathing (when you believe that your breathing is OK) can lead to less oxygen in your brain and reduce brain blood supply by 20-30%.
Our breathing pattern has profound effects on the brain. Unnoticeable changes in breathing (when you believe that your breathing is OK) can lead to less oxygen in your brain and reduce brain blood supply by 20-30%.
How should we breathe, day and night, to ensure maximum oxygenation and cerebral blood flow of the brain? Which breathing pattern is the best for our nervous system? How to get more oxygen to the brain?
While over 95% of people believe that the deep or big breathing pattern is good for health, medical, and physiological evidence (hundreds of publications) provide the opposite answer. Indeed, there is not a single study that confirmed or found that a deep breathing pattern improves or is good for our health. Why?
If you take 100 fast and deep breaths in succession, you can pass out or faint due to a lack of available oxygen for the brain – brain hypoxia. There are dozens of medical studies that confirm this effect.
While we would not recommend it, you can test these ideas practically. If anyone takes repeated deep and fast breaths (hyperventilates), they may pass out (or faint) due to a lack of oxygen in the brain.
The video “How to get more oxygen to your brain?” is on the right side.
Cerebral vasoconstriction is a linear effect – the more you hyperventilate, the more blood vessels in the brain (and other tissues) constrict. Those who hyperventilate (over-breath), have been observed, on average, to have about 20% less oxygen in the brain 24/7. At this level, your brain oxygenation will be in between these two images.
Hyperventilation is a health hazard. Healthy people have light, slow, and shallow breathing pattern and excellent oxygenation. If you observe the breathing of your healthy relatives and friends, you will see nothing and hear nothing.
Sick people (those with asthma, heart disease, bronchitis, cancer, diabetes, depression, fatigue, insomnia, addictions, and many other problems), on the other hand, breathe heavy and, as a result, have a lack of oxygen in the brain as well as low cell oxygen levels. They are hyperventilating.
You can easily measure your maximum brain oxygen content
Use the stress-free breath holding time test. Breathe normally while sitting; after your usual exhale pinch the nose (to prevent slight unconscious breathing), and measure the breath-holding time (in seconds) only until the first distress or discomfort. [Warning. Some, not all, people with heart disease, migraine headaches, and panic attacks may experience negative symptoms minutes later after this light version of the test. If this happens, they should avoid this test.]
The most common mistake is to overdo breath-holding during the test. In this case, you will notice that the stress is gradually increasing. It is time to stop. If you do the test correctly, you will not gasp for air after the test. In fact, your breathing pattern must be exactly the same after the correct test as it was just before it.
What are the typical breath holding time test results?
Severely sick, hospitalized, and terminally ill patients have a breath-holding time of between 1 to 10 s (this is referred to as 1 to 10 s of oxygen). With approaching death, their breathing gets bigger, deeper, and heavier, while breath-holding time approaches zero: 5, 4, 3, 2, and only 1 second just before the death. (You may remember seeing last frantic and dramatic gasps for the air of dying people.)
Sick patients with mild forms of the disease (asthma, heart disease, diabetes, cancer, etc.) have about 10-20 s. These patients are usually on medication to control their symptoms. Asymptomatic asthmatics, heart patients, and many others have slightly more than 20 s of oxygen. (See the links to studies below.)
Healthy adults, according to published western results, should have about 40 s, but a group of Russian MDs practicing the Buteyko holistic self-oxygenation therapy found that 60 s of oxygen is incompatible with about 150 chronic diseases or diseases of civilization. Hence, they established 60 s as the goal of the therapy.
The ideal breathing pattern, which provides the maximum brain with 3 min of oxygen at rest, corresponds to a breathing frequency of only 3-4 breaths per min during basal or unconscious breathing.
What are the causes of maximum brain hypoxia when we overbreathe?
When we breathe heavier or deeper (more than the norm), we remove too much CO2 from all cells of the human organism. This causes:
* Reduced blood flow to the brain. CO2 deficiency causes constriction of blood vessels (arteries and arterioles) and our brains get less blood supply. This physiological fact can be found in many medical textbooks. As Professor Newton from the University of Southern California Medical Center recently reported, “cerebral blood flow decreases 2% for every mm Hg decrease in CO2” (Newton, 2004).
That means that with each second decrease in the oxygenation index, blood flow to the maximum brain is less by about 1%. Less blood means a decreased supply of glucose (the main fuel for the maximum brain in normal conditions), oxygen, and other nutrients. In addition, it causes a gradual accumulation of waste products in tissues.
** The suppressed Bohr effect. As we know, oxygen is transported by hemoglobin containing red blood cells. How do these red blood cells know where in the body to release more oxygen and where less? Why do they unload more oxygen in those places where more is required? Hemoglobin containing red blood cells sense higher concentrations of CO2 and release oxygen in these locations. This effect strongly depends on the absolute CO2 values in the blood and the lungs.
If the CO2 concentration is low, O2 is held tightly on the red blood cells. (Scientists call this effect “increased oxygen affinity to hemoglobin”). Hence, hyperventilation which results in CO2 deficiency leads to hypoxia or low oxygenation of the body cells (the suppressed Bohr effect). The more we breathe at rest, the less the oxygenation of our cells in vital organs like the brain, heart, liver, kidneys, etc.
Not only is the inflow of oxygen less (due to vasoconstriction), but also its release is hampered by low CO2 concentrations (the Bohr effect). That further reduces maximum brain oxygenation.
Do clinical studies show that patients with mental or psychological problems have heavy breathing?
In 1976 the British Journal of Psychiatry published a study of CO2 measurements in 60 patients with neurotic depression and non-retarded endogenous depression (Mora et al, 1976). All patients had abnormally low carbon dioxide values.
Later, in 1990, American psychiatrists from (City University of New York) reported results from several groups of subjects with anxiety, panic phobia, depression, migraine, and idiopathic seizures. The abstract states “virtually all the non-control subjects were found to show moderate to severe hyperventilation and accompanying EEG dysrhythmia” (Fried et al, 1990). In addition, it notes that hyperventilation and abnormal electrical signals in the brain took place simultaneously.
Canadian scientists from the Department of Psychiatry (University of Manitoba, Winnipeg) measured carbon dioxide concentrations in over 20 patients with panic disorder. Their average CO2 was also below the medical norm (Asmundson and Stein, 1994). There are many other studies that report abnormally low CO2 values for people with various psychological and neurological problems.
Is hyperventilation the cause of these health problems?
There is not any evidence showing that people with normal breathing parameters suffer from neurological or psychological problems. All available research indicates that all patients with depression, schizophrenia, phobias, panic attacks, ADD, ADHD, addictions, sleeping problems, etc. have abnormal breathing pattern manifested in chronic hyperventilation.
This suggests that hyperventilation is (at least partially) a cause of, rather than a result of, these conditions.
How to get maximu Brain oxygen?
If you normalize your breathing, your breath holding time will be about 40-60 s (corresponding to abundant oxygen in the body and the brain), and your health problems related to the brain or the central nervous system will disappear. Russian Doctor KP Buteyko, MD developed the medical self-oxygenation therapy known as “the Buteyko method”.
He trained about 200 MDs to use the Buteyko oxygenation therapy in practice. The prime goal of this therapy is to normalize breathing and body oxygenation. Normal breathing is invisible and inaudible. It is light and relaxed: we take tiny or small inhalation and immediately relax for a longer exhalation, then again we take a small inhalation. Normal breathing provides the human body with superior oxygenation and naturally eliminates many chronic conditions.
You can find a short summary of key lifestyle factors that provide improved maximum brain oxygenation. These factors are summarized in the Table that is provided right below here as your bonus content.
Healthy lifestyle factors– Physical exercise with strictly nasal breathing |
Lifestyle risk factors– Lack of physical exercise |
[/sociallocker]
For references click here: References. This article about how to get more oxygen to the maximum brain was created in 2009. Since then, we accumulated 100s of clinical results related to awful breathing in modern people. For updated resources and new clinical findings, visit the Homepage of this site.
Below are authentic comments, questions, and testimonials from the same page on the old PHP site before we converted it to WordPress.
On 2018-04-21T08:52:32, Dr. Artour (mod) wrote:
It is complex because factors work in opposite directions. Reduced breathing can very lightly decrease SpO2, but diaphragmatic breathing improves it, while vaso-effects contribute depending on the state of the nervous system. Generally, yes, students with easier breathing have a little less SpO2.
On 2018-04-20T13:32:35, Murray McEwan wrote:
If monitoring SpO2 with a fingertip oximeter while resting, a reading of 92 indicates better oxygenation than 97, but so far as optimizing the CO2 level, is the lower SpO2 reading actually indicative of a better CO2:O2 balance, or is there no direct correlation?
On 2018-02-26T08:45:35, Dr. Artour (mod) wrote:
The degree of IQ increase is very individual and also depends on initial symptoms and states.
On 2018-02-26T01:48:50, Dallas wrote:
Will increasing my body oxygen level also increase intelligence/IQ. If so by how much will my IQ increase estimation) if I reach 40-60s on body oxygen test.
On 2017-09-03T07:36:53, Dr. Artour (mod) wrote:
It is common for people with less than 20 s morning CP, but very rare among healthy people.
On 2017-09-02T17:52:00, Endrju Gelara wrote:
After waking up, usually one of my nostrils is partially congested, is that normal?
On 2017-09-02T05:16:17, Dr. Artour (mod) wrote:
Unlikely to help without lifestyle changes.
On 2017-09-02T02:28:22, Jan Kowalski wrote:
Some coaches encourage trainees to breathe faster during strength training to failure, the usual recommendation is to breathe continuously and naturally with an open mouth. As the exercise becomes more difficult causing the burning sensation in the muscles, one should deliberately breathe faster or hyperventilate – this type of breathing would supposedly blow off CO2 carbon dioxide) and keep your blood pH normal longer. It shall allow your muscles to function for a longer duration and therefore inroad more deeply. In my experience, it only resulted in dizziness. For the last few months, I tried inhaling through the nose and exhaling through the mouth during such workouts, but my body oxygenation didn’t improve, I can hold my breath for about 30 sec at rest. Now I’m trying to breathe only through the nose when training – will I get used to that eventually and will it contribute to increasing the time for breath-holding? Also, is it going to improve my breathing patterns just like limiting breathing during endurance training and breath-holding exercises, etc.? Thanks for your feedback.
On 2017-09-01T10:45:32, Dr. Artour (mod) wrote:
Only through the nose and, if possible, less.
On 2017-09-01T01:34:18, Jan Kowalski wrote:
How would you recommend to breathe during high-intensity strength training performing sets to momentary muscular failure) or high-intensity interval training?
On 2016-06-20T15:00:34, Anonymous wrote:
good
On 2015-07-22T15:32:13, Artour (mod) wrote:
There are old studies that calculated O2 in the alveoli, up to 100 years old. I have not seen any recent studies, but they might exist.
Since you did not specify exactly where you want to know the O2 value lungs, blood, tissues), this means that you do not have a clear vision of what you are looking for.
On 2015-07-21T21:16:21, Mario Balczar wrote:
I have a very important question, I need the answer to a scientific article. Which is the oxygen concentration after 20 seconds of air retention? I hope the answer. Thank you!!
On 2013-04-30T06:17:05, Artour (mod) wrote:
For over a decade, I teach students how to increase this breath-holding time up to 30-40 and sometimes over 60 s. This article is very old in comparison with the rest of the site.
On 2013-04-30T03:22:11, Anonymous wrote:
you have to be mistaken. no one can operate without distress for 40 seconds after exhaling: you exhaled all the air in your lungs are essentially running on nothing. discomfort comes soon enough 1-10s) normally. perhaps you mean inhale?

