- Updated on August 3, 2021
When a person starts to overbreathe or hyperventilate (breathe more air per minute), blood oxygenation in the lungs has negligible changes. Why? During normal breathing hemoglobin cells of the arterial blood have 98-99% O2 saturation. Hence, big breathing cannot increase blood oxygenation in any significant degree.
What are the other effects, if a healthy person starts to breathe more or deeper?
– More carbon dioxide is removed from the lungs with each breath and therefore the level of CO2 in the lungs immediately decreases.
– In 1-2 minutes, the CO2 level falls below the normal levels in all the blood due to its circulation.
– In 3-5 minutes most cells of the body (including vital organs and muscles) due to CO2 diffusion experience lowered CO2 concentrations;
– In 15-20 minutes, the CO2 level in the brain is below the norm due to a slower diffusion rate.
A. Vasodilation-vasoconstriction effect
Hypocapnia (low CO2 concentration in the arterial blood) reduces perfusion of the following organs:
– heart (Hoffman et al, 2001; Coetzee et al, 1984; Fox et al, 1979; Karlsson et al, 1994; Wexels et al, 1985; Okazaki et al, 1991; Okazaki et al, 1992),
– brain (Fortune et al, 1995; Karlsson et al, 1994; Hoffman et al, 2001; Liem et al, 1995; Starling & Evans, 1968; Tsuda et al, 1987; Macey et al, 2007; Santiago & Edelman, 1986),
– kidneys (Karlsson et al, 1994; Okazaki, 1989),
– spleen (Karlsson et al, 1994),
– liver (Hughes et al, 1979; Dutton et al, 1976; Fujita et al, 1989; Okazaki, 1989),
– colon (Gilmour et al, 1980).
For abstracts, visit the main page related to CO2 vasodilation-vasoconstriction effect.
What is the cause of the reduced blood flow to vital organs? CO2 is a dilator of arteries and arterioles. These blood vessels have tiny smooth muscles around them that can constrict or dilate depending on carbon dioxide concentrations. When we breathe more, CO2 level becomes smaller in the arterial blood; these blood vessels constrict; and vital organs (like the heart, brain, liver, stomach, kidneys, colon, spleen, etc.) get less blood supply.
Personal observations
Imagine that any person starts to hyperventilate voluntarily at rest (fast and deep breathing). What should happen with this person? He would feel dizzy and could easily faint or pass out. Why? It cannot be due to too much oxygen, since their blood is almost completely saturated with oxygen during very shallow (or normal) breathing at rest.
This scan below shows brain oxygen content in two conditions: normal breathing and after 1 minute of deliberate hyperventilation. The red color represents the most O2, dark blue the least. Brain oxygenation after 1 minute if overbreathing is lowered by about 40%. (Litchfield, 2003).
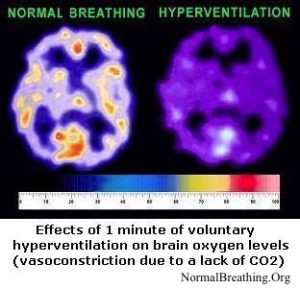
This finding is quoted in medical textbooks (e.g., Starling & Evans, 1968) since it has been confirmed by dozens of professional studies. According to the Handbook of Physiology (Santiago & Edelman, 1986), “cerebral blood flow decreases 2% for every mm Hg decrease in CO2” pressure.
Be observant. When you get a mall bleeding cut or a wound, deliberately hyperventilate and see if that can help stop the bleeding. It should happen. As an alternative, perform comfortable breath holding and breathe less and accumulate CO2. What would happen with your bleeding? (It should increase.) Now you know what to do after dental surgeries, brain traumas, and other accidents involving bleeding. It is natural for humans and other animals to breathe heavily in such conditions. Hence, hyperventilation can be life saving in cases of severe bleeding.
B. The Bohr effect
The description of the Bohr law (discovered over a century ago) can be found in standard physiological textbooks since it was confirmed by dozens of professional studies (e.g., Braumann et al, 1982; Boning et al, 1975; Bucci et al, 1985; Carter et al, 1985; diBella et al, 1986; Dzhagarov et al, 1996; Grant et al, 1982; Grubb et al, 1979; Gersonde et al, 1986; Hlastala & Woodson, 1983; Jensen, 2004; Kister et al, 1988; Kobayashi et al, 1989; Lapennas, 1983; Matthew et al, 1979; Meyer et al, 1978; Tyuma, 1984; Winslow et al, 1985). These references and their abstracts can be found on the Bohr effect webpage.
What is the Bohr effect? As we know, oxygen is transported in the blood by hemoglobin cells. How do these red blood cells know where to release more oxygen and where less is needed? Or why do they unload more oxygen in those places where more is required? For example, at rest the heart muscle requires more oxygen, but blood travels everywhere.
The hemoglobin cells sense higher concentrations of CO2 (end product of energy production) and release oxygen in such places. The effect strongly depends on the absolute CO2 values in the blood and the lungs.
If the CO2 concentration is low, O2 cells are stuck to the red blood cells. Hence, CO2 deficiency leads to hypoxia or low oxygenation of the body cells (the suppressed Bohr effect). The more we breathe at rest, the less the oxygenation of our cells in the vital organs, like brain, heart, liver, kidneys, etc.
The Bohr effect is crucial for our survival. Why? At each moment of our lives, some organs and tissues work harder and produce more CO2. These additional CO2 concentrations are sensed by the hemoglobin cells and cause them to release more O2 in those places where it is most required. This is a smart self-regulating mechanism for efficient O2 transport.
For example, without the Bohr effect, you could not walk or run even for 3-5 minutes. Why? In normal conditions, due to the Bohr effect, more O2 is released by red blood cells in those muscles, which generate more CO2. Hence, these muscles will get more O2 and can continue to work with the same high rate.
Western studies confirmed that hyperventilation reduces oxygenation tension (or oxygen availability) in vital organs, including:
– brain (Coetzee et al, 1984; Hoffman et al, 2001; Liem et al, 1995; Tsuda et al, 1987),
– heart (Coetzee et al, 1984; Fox et al, 1979; Hashimoto et al, 1989; Hoffman et al, 2001; Okazaki et al, 1991; Okazaki et al, 1992; Wexels et al, 1985),
– liver (Okazaki et al, 1989),
– kidneys (Hughes et al, 1979; Okazaki et al, 1989).
But we already considered that cancer patients breathe much more than the norm and, indeed, their heavy breathing increases their mortality rates. Now we can explain what happens with their cell oxygenation when they breathe faster or more.
References
Coetzee A, Holland D, Fox P, Ryder A, Jones L, The effect of hypocapnia on coronary blood flow and myocardial function in the dog, Anesthesia and Analgesia 1984 Nov; 63(11): p. 991-997.
Dutton R, Levitzky M, Berkman R, Carbon dioxide and liver blood flow, Bull Eur Physiopathol Respir. 1976 Mar-Apr; 12(2): p. 265-273.
Gilmour DG, Douglas IH, Aitkenhead AR, Hothersall AP, Horton PW, Ledingham IM, Colon blood flow in the dog: effects of changes in arterial carbon dioxide tension, Cardiovasc Res 1980 Jan; 14(1): p. 11-20.
Fox P, Ryder WA, Effect of CO2 on the systemic and coronary circulations and on coronary sinus blood gas tensions, Bull Eur Physiopathol Respir 1979 Jul-Aug; 15(4): p.625-638.
Fortune JB, Feustel PJ, deLuna C, Graca L, Hasselbarth J, Kupinski AM, Cerebral blood flow and blood volume in response to O2 and CO2 changes in normal humans, J Trauma. 1995 Sep; 39(3): p. 463-471.
Fujita Y, Sakai T, Ohsumi A, Takaori M, Effects of hypocapnia and hypercapnia on splanchnic circulation and hepatic function in the beagle, Anesthesia and Analgesia 1989 Aug; 69(2): p. 152-157.
Hashimoto K, Okazaki K, Okutsu Y, The effects of hypocapnia and hypercapnia on tissue surface PO2 in hemorrhaged dogs [Article in Japanese], Masui 1989 Oct; 38(10): p. 1271-1274.
Henderson Y, Acapnia and shock. – I. Carbon dioxide as a factor in the regulation of the heart rate, American Journal of Physiology 1908, 21: p. 126-156.
Hoffman WE, Albrecht RF 2nd, Ripper R, Jonjev ZS, Brain compared to heart tissue oxygen pressure during changes in arterial carbon dioxide in the dog, J Neurosurg Anesthesiol. 2001 Oct; 13(4): p.303-309.
Hughes RL, Mathie RT, Fitch W, Campbell D, Liver blood flow and oxygen consumption during hypocapnia and IPPV in the greyhound, J Appl Physiol. 1979 Aug; 47(2): p. 290-295.
Karlsson T, Stjernstrom EL, Stjernstrom H, Norlon K, Wiklund L, Central and regional blood flow during hyperventilation. An experimental study in the pig, Acta Anaesthesiol Scand. 1994 Feb; 38(2): p.180-186.
Liem KD, Kollee LA, Hopman JC, De Haan AF, Oeseburg B, The influence of arterial carbon dioxide on cerebral oxygenation and haemodynamics during ECMO in normoxaemic and hypoxaemic piglets, Acta Anaesthesiol Scand Suppl. 1995; 107: p.157-164.
Litchfield PM, A brief overview of the chemistry of respiration and the breathing heart wave, California Biofeedback, 2003 Spring, 19(1).
Macey PM, Woo MA, Harper RM, Hyperoxic brain effects are normalized by addition of CO2, PLoS Med. 2007 May; 4(5): e173.
McArdle WD, Katch FI, Katch VL, Essentials of exercise physiology (2nd edition); Lippincott, Williams and Wilkins, London 2000.
Okazaki K, Okutsu Y, Fukunaga A, Effect of carbon dioxide (hypocapnia and hypercapnia) on tissue blood flow and oxygenation of liver, kidneys and skeletal muscle in the dog, Masui 1989 Apr, 38 (4): p. 457-464.
Okazaki K, Hashimoto K, Okutsu Y, Okumura F, Effect of arterial carbon dioxide tension on regional myocardial tissue oxygen tension in the dog [Article in Japanese], Masui 1991 Nov; 40(11): p. 1620-1624.
Okazaki K, Hashimoto K, Okutsu Y, Okumura F, Effect of carbon dioxide (hypocapnia and hypercapnia) on regional myocardial tissue oxygen tension in dogs with coronary stenosis [Article in Japanese], Masui 1992 Feb; 41(2): p. 221-224.
Santiago TV & Edelman NH, Brain blood flow and control of breathing, in Handbook of Physiology, Section 3: The respiratory system, vol. II, ed. by AP Fishman. American Physiological Society, Betheda, Maryland, 1986, p. 163-179.
Starling E & Lovatt EC, Principles of human physiology, 14-th ed., 1968, Lea & Febiger, Philadelphia.
Tsuda Y, Kimura K, Yoneda S, Hartmann A, Etani H, Hashikawa K, Kamada T, Effect of hypocapnia on cerebral oxygen metabolism and blood flow in ischemic cerebrovascular disorders, Eur Neurol. 1987; 27(3): p.155-163.
Wexels JC, Myhre ES, Mjos OD, Effects of carbon dioxide and pH on myocardial blood-flow and metabolism in the dog, Clin Physiol. 1985 Dec; 5(6): p.575-588.

