- Updated on August 7, 2019
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
Do not expect your CF doctor to know any of these things since modern medical schools teach zero information about breathing in the real world and breathing retraining. Doctors are commonly not educated even in basics of key lifestyle factors for health, such as diet, sleep, and exercise.
In this YouTube video below, Dr. Artour Rakhimov explains how cystic fibrosis develops in the lungs and GI tract, and how breathing retraining, according to the amazing experience of Soviet Buteyko doctors and his students, can reverse cystic fibrosis naturally.
 People with cystic fibrosis in lungs destroy their alveoli and airways due to their chronic hyperventilation. Overbreathing is a norm in cystic fibrosis (see the table below). There are several mechanisms that are responsible for deleterious effects of hyperventilation on the lung tissue.
People with cystic fibrosis in lungs destroy their alveoli and airways due to their chronic hyperventilation. Overbreathing is a norm in cystic fibrosis (see the table below). There are several mechanisms that are responsible for deleterious effects of hyperventilation on the lung tissue.
Effects of hyperventilation on lungs
While studying the effects of CO2 (carbon dioxide) on lung tissue a large group of scientists from the Lung Biology Program, The Research Institute and Department of Critical Care Medicine and Anesthesia, (University of Toronto, Ontario, Canada) concluded that “CO2 modulates key physiologic indices of lung injury, including alveolar-arterial oxygen gradient and airway pressure, indicating a potential role in the pathogenesis of ventilator-associated lung injury. These effects are surfactant independent.” (Laffey et al, 2003).
Minute ventilation in cystic fibrosis patients at rest
| Condition | Minute ventilation |
Number of patients |
References |
| Normal breathing | 6 L/min | – | Medical textbooks |
| Healthy subjects | 6-7 L/min | >400 | Results of 14 studies |
| Cystic fibrosis | 15 L/min | 15 | Fauroux et al, 2006 |
| Cystic fibrosis* | 13 (�2) L/min | 10 | Bell et al, 1996 |
| Cystic fibrosis | 10 L/min | 11 | Browning et al, 1990 |
| Cystic fibrosis | 11-14 L/min | 6 | Tepper et al, 1983 |
| Cystic fibrosis* | 10 L/min | 10 | Ward et al, 1999 |
| CF and diabetes* | 10 L/min | 7 | Ward et al, 1999 |
| Cystic fibrosis | 16 L/min | 7 | Dodd et al, 2006 |
| Cystic fibrosis | 18 L/min | 9 | McKone et al, 2005 |
Click here for all Cystic Fibrosis References
Effects of whole-body hypoxia on lungs
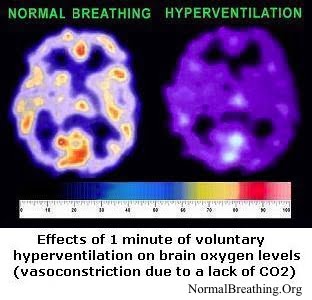 Studies showed that the transport of ions of Na and Cl, and water in the epithelium layers of the lungs depend on oxygen levels (Clerici & Matthay, 2000; Karle et al, 2004; Mairbaurl et al, 1997; Mairbaurl et al, 2002 – these references can be found on other CF pages). This effect is present in all mammals. What about cystic fibrosis-related research? Several medical studies found that the function of the CFTR (cystic fibrosis transmembrane conductance regulator) gene is directly influenced by body-oxygen levels, which define concentrations of hypoxia-inducible factor-1 (Bebk et al, 2001; Guimbellot et al, 2008; Yeger et al, 2001; Zheng et al, 2009 – these references are also provided on other CF pages).
Studies showed that the transport of ions of Na and Cl, and water in the epithelium layers of the lungs depend on oxygen levels (Clerici & Matthay, 2000; Karle et al, 2004; Mairbaurl et al, 1997; Mairbaurl et al, 2002 – these references can be found on other CF pages). This effect is present in all mammals. What about cystic fibrosis-related research? Several medical studies found that the function of the CFTR (cystic fibrosis transmembrane conductance regulator) gene is directly influenced by body-oxygen levels, which define concentrations of hypoxia-inducible factor-1 (Bebk et al, 2001; Guimbellot et al, 2008; Yeger et al, 2001; Zheng et al, 2009 – these references are also provided on other CF pages).
 Tissue hypoxia is a normal outcome of hyperventilation (see links to hundreds of studies below). Do people with cystic fibrosis hyperventilate? Consider minute ventilation (how many liters per minute the person inhales) at rest in cystic fibrosis patients.
Tissue hypoxia is a normal outcome of hyperventilation (see links to hundreds of studies below). Do people with cystic fibrosis hyperventilate? Consider minute ventilation (how many liters per minute the person inhales) at rest in cystic fibrosis patients.
Find more details in this YouTube video – Trailer of the Amazon Kindle Book “Cystic Fibrosis Life Expectancy”.
Hyperventilation and mouth breathing causes drying and overcooling of airways
What are the effects of habitual mouth breathing and hyperventilation? One study measured the effects of the breathing route on humidity and surface temperature in airways of normal and CF subjects. During nose breathing, the nasal passages can humidify and warm up the incoming flow of air. Mouth breathing leads to the drying and cooling of airways. For example, during inspiration, the humidity at the pharynx for nose breathing was about 95%, while for oral breathing it was only 75% (Primiano et al, 1988). Hence, mouth breathing requires 5 times more water from bronchi and bronchioles in order to achieve 100% humidity. These doctors observed that, “… These data suggest that when the rate of evaporation is sufficiently high, the rate-limiting step may be water transport through the mucosal tissue and/or secretions. At least for the upper airways, this rate limitation is more evident for CF patients than for normal subjects.”
 An additional effect of hyperventilation relates to the overcooling of airways, especially in cases of mouth breathing and coughing through the mouth. Even stronger effects are expected due to physical exercise with mouth breathing. All physical activity in patients with cystic fibrosis must be done with nose breathing only (in and out).
An additional effect of hyperventilation relates to the overcooling of airways, especially in cases of mouth breathing and coughing through the mouth. Even stronger effects are expected due to physical exercise with mouth breathing. All physical activity in patients with cystic fibrosis must be done with nose breathing only (in and out).
While measuring the temperature of airways during pulmonary and hyperventilation tests, a group of Italian doctors discovered that hyperventilation induced a significant temperature loss (Vitacca et al, 1994). The aim of their study was to test the usefulness of hygroscopic humidifiers on the secretion of mucus and on an inspired gas temperature in tracheostomized patients. These Italian doctors found that hygroscopic condenser humidifiers have positive effects on the thickness and coloring of mucosal secretions: “Statistically significant differences were found in thickness and coloring of secretions between the two groups during the period of 10 days. Group 2 showed a significantly greater trend in the number of bacteria than Group 1. The group with the hygroscopic condenser humidifier showed respiratory function improvement over time for forced expiratory volume in one second (FEV1) and tidal volume (VT), maximal inspiratory pressure (MIP), and maximal voluntary ventilation (MVV) in comparison to the control group, who did not.” In conclusions, they wrote that hygroscopic condenser humidifiers can be useful, among other things, to “heat inspiratory airflow, possibly protecting against temperature loss during a hyperventilation test”.
These results suggest that chronic hyperventilation in cystic fibrosis also leads to overcooling of airways. In addition, even a slight drop in temperatures of airways can lead to immune dysfunction and possible respiratory infections. Overcooling may also contribute to thickness and coloring of sputum, as the above study suggested. All these effects worsen cystic fibrosis in the lungs.
Other effects of overbreathing on the development of cystic fibrosis and problems in the lungs
 As we discovered before, CO2 dilates airways (see links below). Furthermore, reduced CO2 in airways and reduced oxygenation of the cells will suppress the immune system. Medical studies have found that low CO2 in airways prevents the repair of lung tissue.
As we discovered before, CO2 dilates airways (see links below). Furthermore, reduced CO2 in airways and reduced oxygenation of the cells will suppress the immune system. Medical studies have found that low CO2 in airways prevents the repair of lung tissue.
Chronic overbreathing creates cell hypoxia and, hence, suppresses the immune system due to the production of free radicals and cellular damage, as well as abnormalities in the metabolism of proteins. It is logical then that heavy and fast breathing in cystic fibrosis patients leads to the typical symptoms and features of chronic alveolar hyperventilation, including frequent infections of airways, coughing, pneumothorax, bouts of bronchitis, sinusitis, and pneumonia, diarrhea, foul-smelling, greasy stools, severe constipation, rectal prolapse, liver disease, pancreatitis, diabetes, gallstones, and infertility.
Cystic fibrosis in lungs and clinical experience of Russian MDs
 Over 170 Soviet and Russian medical doctors found that cystic fibrosis in the lungs is reversible with breathing normalization. Meanwhile, people with cystic fibrosis can retrain their breathing and learn how to breathe differently 24/7 or they are able to change their breathing pattern using direct means (e.g., diaphragmatic breathing exercises and strictly nasal breathing during physical exercise) and indirect techniques (like taping one’s mouth at night, prevention of sleeping on one’s back, correct posture 24/7, normal thermo-exchange, etc.). To achieve over 20 seconds for the morning body-oxygen test is the crucial first step to prevent and reverse main problems with cystic fibrosis in lungs. By the way, these Russian doctors do not teach silly forceful coughing techniques for the removal of mucus since it worsens cystic fibrosis in lungs. (Such coughing techniques are still used by many medical professionals.)
Over 170 Soviet and Russian medical doctors found that cystic fibrosis in the lungs is reversible with breathing normalization. Meanwhile, people with cystic fibrosis can retrain their breathing and learn how to breathe differently 24/7 or they are able to change their breathing pattern using direct means (e.g., diaphragmatic breathing exercises and strictly nasal breathing during physical exercise) and indirect techniques (like taping one’s mouth at night, prevention of sleeping on one’s back, correct posture 24/7, normal thermo-exchange, etc.). To achieve over 20 seconds for the morning body-oxygen test is the crucial first step to prevent and reverse main problems with cystic fibrosis in lungs. By the way, these Russian doctors do not teach silly forceful coughing techniques for the removal of mucus since it worsens cystic fibrosis in lungs. (Such coughing techniques are still used by many medical professionals.)
References: CO2 and cystic fibrosis in lungs
Laffey JG, Engelberts D, Duggan M, Veldhuizen R, Lewis JF, Kavanagh BP, Carbon dioxide attenuates pulmonary impairment resulting from hyperventilation, Crit Care Med. 2003 Nov;31(11):2634-40.
Laffey JG, Engelberts D, Kavanagh BP, Injurious effects of hypocapnic alkalosis in the isolated lung, Am J Respir Crit Care Med. 2000 Aug;162(2 Pt 1):399-405.
Ward SA, Tomezsko JL, Holsclaw DS, Paolone AM, Energy expenditure and substrate utilization in adults with cystic fibrosis and diabetes mellitus, Am J Clin Nutr 1999;69:913–9.
Brigitte Fauroux, Fr´ed´eric Nicot, Pierre-Yves Boelle, Mich`ele Boul´e, Annick Cl´ement, Fr´ed´eric Lofaso, Monique Bonora, Mechanical limitation during CO2 rebreathing in young patients with cystic fibrosis, Respiratory Physiology & Neurobiology 153 (2006) 217–225
Jonathan D. Dodd, Sinead C. Barry, Charles G. Gallaghe, Respiratory factors do not limit maximal symptom-limited exercise in patients with mild cystic fibrosis lung disease, Respiratory Physiology & Neurobiology 152 (2006) 176–185
, Browning IB, D’Alonzo GE, Tobin MJ, Importance of respiratory rate as an indicator of respiratory dysfunction in patients with cystic fibrosis, Chest. 1990 Jun;97(6):1317-21.

