- Updated on September 13, 2020
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
- Medically Reviewed by Naziliya Rakhimova, MD
Bronchoconstriction Causes and Natural CO2-Based Treatment
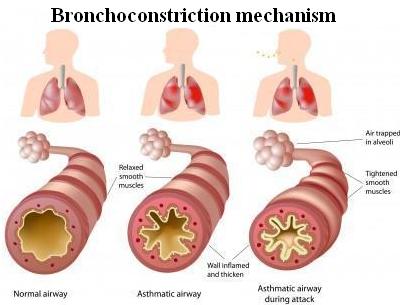 Bronchoconstriction (definition) is defined as the narrowing of the airways in the lungs (bronchi and bronchioles). Airflow in air passages can get restricted due to 3 factors:
Bronchoconstriction (definition) is defined as the narrowing of the airways in the lungs (bronchi and bronchioles). Airflow in air passages can get restricted due to 3 factors:
– a spasmodic state of the smooth muscles in bronchi and bronchioles
– an inflammation of the airways
– excessive production of mucus due to an allergic reaction or irritation caused by mechanical friction of air (due to shear stress), overcooling or drying of airways.
Bronchoconstriction is common in people with respiratory problems, such as asthma, COPD, and cystic fibrosis. Medical sources continue to misinform public about the true causes of bronchoconstriction.
This YouTube video features Dr. Artour Rakhimov who explains causes of bronchoconstriction and its treatment.
Here are clinical facts.
Ventilation rates (chronic diseases)
| Condition | Minute ventilation |
Number of people |
All references or click below for abstracts |
| Normal breathing | 6 L/min | – | Medical textbooks |
| Healthy Subjects | 6-7 L/min | >400 | Results of 14 studies |
| Asthma | 13 (+-2) L/min | 16 | Chalupa et al, 2004 |
| Asthma | 15 L/min | 8 | Johnson et al, 1995 |
| Asthma | 14 (+-6) L/min | 39 | Bowler et al, 1998 |
| Asthma | 13 (+-4) L/min | 17 | Kassabian et al, 1982 |
| Asthma | 12 L/min | 101 | McFadden, Lyons, 1968 |
| COPD | 14 (+-2) L/min | 12 | Palange et al, 2001 |
| COPD | 12 (+-2) L/min | 10 | Sinderby et al, 2001 |
| COPD | 14 L/min | 3 | Stulbarg et al, 2001 |
| Cystic fibrosis | 15 L/min | 15 | Fauroux et al, 2006 |
| Cystic fibrosis | 10 L/min | 11 | Browning et al, 1990 |
| Cystic fibrosis* | 10 L/min | 10 | Ward et al, 1999 |
| CF and diabetes* | 10 L/min | 7 | Ward et al, 1999 |
| Cystic fibrosis | 16 L/min | 7 | Dodd et al, 2006 |
| Cystic fibrosis | 18 L/min | 9 | McKone et al, 2005 |
| Cystic fibrosis* | 13 (+-2) L/min | 10 | Bell et al, 1996 |
| Cystic fibrosis | 11-14 L/min | 6 | Tepper et al, 1983 |
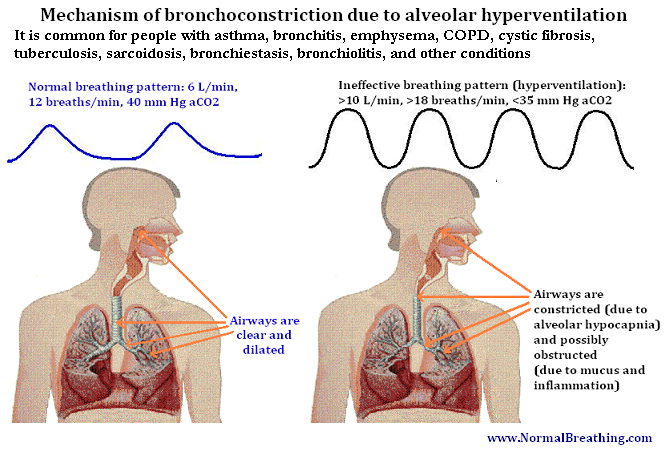
As a result of heavy breathing, all these people suffer from alveolar hypocapnia (lack of CO2 in airways).
Cause of bronchoconstriction
It is a known physiological law that all smooth muscles are highly sensitive to CO2 levels. Thus, spasm in the smooth muscles of bronchi and bronchioles is a normal physiological reaction to alveolar hyperventilation (Badier et al, 1998; Clarke et al, 1982; Jamison et al, 1987; O’Cain et al, 1979; Sterling, 1968).
While there are many chemicals that can cause either bronchoconstriction or bronchodilation, CO2 plays the key role due to two factors: its high bronchodilatory potency and additional negative systemic effects caused by alveolar hypocapnia (lack of CO2). What are those?
Chronic hyperventilation (breathing more air than the medical norm) also leads to cell hypoxia, generation of reactive oxygen species (free radicals), and immunosuppression. (This can happen with or without ventilation-perfusion mismatch: blood CO2 levels can be below the norm or too high.)
As a result, overbreathing produces additional effects that worsen conductivity of airways, such as immunosuppression, frequent respiratory infections, excessive production of sputum (mucus) and airway inflammation (see links to studies below).
Furthermore, overbreathing also leads to increased losses of water from the mucosal layers of airways and overcooling of airways due to increased heat losses. These effects also favor frequent respiratory infections.
Symptoms of bronchoconstriction
 These effects cause further airway obstruction, difficulty breathing, wheezing, coughing, and dyspnea (shortness of breath) amplifying the effects of bronchoconstriction.
These effects cause further airway obstruction, difficulty breathing, wheezing, coughing, and dyspnea (shortness of breath) amplifying the effects of bronchoconstriction.
Causes and mechanism of bronchoconstriction
Consider medical evidence related to breathing parameters at rest in people with bronchoconstriction (see the Table above). We see that these patients breathe at rest (in stable conditions) much more air than the medical norm. Over breathing leads to low CO2 in the airways and causes other effects summarized here.
Bronchoconstriction can also happen due to an allergic reaction caused by the release of histamine. This allergic reaction leads to edema and inflammation of airways, as often happens in people with asthma, bronchitis, emphysema, and other COPD-related conditions. However, chronic hyperventilation causes immune dysfunction, and, therefore, it also promotes the appearance of allergies.
Since cell hypoxia promotes chronic inflammation, people with these health conditions (asthma, bronchitis, and so on), as well as people with cystic fibrosis, tuberculosis, sarcoidosis, bronchiectasis, bronchiolitis, and many other lung diseases, experience chronic spasm in the smooth muscles of airways or bronchoconstriction, combined with other negative effects caused by hypocapnia.
This YouTube video explains the cause of bronchoconstriction.
Note about coughing. Coughing through the mouth multiplies all these negative effects of hyperventilation several folds. There are effective breathing techniques how to suppress coughing.
Treatment of bronchoconstriction
 Six most effective clinical controlled trials on asthma cannot be wrong. They achieved 90% reduction in main asthma medication that is used to produce … bronchodilation. In other words, asthmatics can reduce their main symptom (spasm of airways) with a simple natural reduced breathing exercise based on increasing CO2 levels in the lungs and airways.
Six most effective clinical controlled trials on asthma cannot be wrong. They achieved 90% reduction in main asthma medication that is used to produce … bronchodilation. In other words, asthmatics can reduce their main symptom (spasm of airways) with a simple natural reduced breathing exercise based on increasing CO2 levels in the lungs and airways.
What are the origins of this technique? Over 170 Russian medical doctors found an effective way to deal with bronchoconstriction. This medical treatment is based on the restoration of normal alveolar CO2 levels naturally or using willpower. The Buteyko method is approved by the Russian Ministry of Health and has been applied on more than 200,000 people with health problems that involve bronchoconstriction (such as asthma, bronchitis, COPD, cystic fibrosis and many others). According to these Russian doctors, patients need to slow down their heavy breathing and achieve more than 20 s for the body-oxygen test to prevent symptoms of bronchoconstriction at rest. Nose breathing during exercise is crucial since it prevents exercise-induced asthma.
However, we tested the Buteyko technique and compared it with other respiratory techniques. There are methods that are even better than the legendary Buteyko technique to reduce constriction of airways and defeat common respiratory diseases, such as asthma, bronchitis, COPD, emphysema, cystic fibrosis, and others. You can find the names of these great methods right below here as your bonus content.
Breathing exercises with breathing devices (such as the Frolov breathing device, DIY breathing device, and Samozdrav) are very effective ways to increase body oxygen levels and treat bronchoconstriction.
[/sociallocker]
Lifestyle changes are also necessary to prevent overbreathing due to sleep (supine sleep and mouth breathing), meals (overeating), exercise, and other factors.
Medical references
Badier M, Beaumont D, Orehek J,Attenuation of hyperventilation-induced bronchospasm by terfenadine: a new antihistamine, J Allergy Clin Immunol. 1988 Feb;81(2):437-40.
Clarke PS, Jarrett RG, Hall GJ,The protective effect of ipratropium bromide aerosol against bronchospasm induced by hyperventilation and the inhalation of allergen, methacholine and histamine, Ann Allergy. 1982 Mar;48(3):180-3.
Jamison JP, Glover PJ, Wallace WF,Comparison of the effects of inhaled ipratropium bromide and salbutamol on the bronchoconstrictor response to hypocapnic hyperventilation in normal subjects, Thorax. 1987 Oct; 42(10): 809-14.
O’Cain CF, Hensley MJ, McFadden ER Jr, Ingram RH Jr,Pattern and mechanism of airway response to hypocapnia in normal subjects,J Appl Physiol. 1979 Jul;47(1):8-12.
Reynolds AM, McEvoy RD,Tachykinins mediate hypocapnia-induced bronchoconstriction in guinea pigs, J Appl Physiol. 1989 Dec;67(6):2454-60.
Sterling GM,The mechanism of bronchoconstriction due to hypocapnia in man,Clinical Science 1968 Apr; 34(2): p. 277-285.
Straub NC, Section V,The Respiratory System, inPhysiology, edited by. Berne RM & Levy MN, 4th edition, Mosby, St. Louis, 1998.

